Peripheral Nerve Surgery
Peripheral nerve surgery treats nerves outside the brain and spinal cord after they have left the bony protection of the skull and spinal column. Peripheral nerve surgery may be performed by orthopaedic surgeons or plastic surgeons with appropriate training; some neurosurgeons also specialise in this field. I received specific specialist training from Professor David Chwei-Chin Chuang (莊垂慶), a world authority on peripheral nerve and brachial plexus reconstruction from Taiwan, and Professor Susan Mackinnon, a world authority on nerve transfers and treatment of nerve pain from St Louis, Missouri. Most peripheral nerve surgery is done to treat nerve injuries, nerve compression (also called nerve entrapment), and nerve tumours.
Complex peripheral nerve problems are best treated by a team of different specialists, including surgeons, physiotherapists, pain specialists, radiologists and psychologists. I work closely with my colleague, Mr Dean Boyce, at the Welsh Peripheral Nerve Surgery Unit in Morriston Hospital, Swansea, where we run multidisciplinary clinics to manage the most complex injuries in a holistic way.
Nerve injury
Depending on the nerve involved a nerve injury or nerve damage may cause numbness of a patch of skin, paralysis of muscles, or a combination of both. Some patients also experience severe pain from a nerve injury, which can be difficult to treat. The treatment required depends on the severity of the nerve damage.
Neurapraxia
The mildest form of nerve damage, called neurapraxia, recovers on its own. The nerve may be bruised, causing it to stop conducting electrical signals. Since no nerve fibres have been cut, once the nerve starts conducting signals again everything returns to normal. The process of recovery takes anything from a few days to 3 months.
Axonotmesis
With more severe nerve injuries, nerve fibres are damaged. This is called axonotmesis, and can occur after a severe crush, stretch or partial cut of a nerve. In order to get any recovery, the damaged nerve fibres have to regrow from where they were injured back to the muscle or patch of skin that they supply. This takes a long time because nerves only grow 1 millimetre per day (around 1 inch per month).
If the microscopic tubes that surround each nerve fibre haven’t been injured, there is a good chance that most nerve fibres will reach their targets and a near-full recovery can be expected – even without surgery. However, if the tubes have also been injured, regenerating nerve fibres can lose their way, may grow down the wrong tubes or get trapped in scar tissue at the site of the injury.
Neurotmesis
The worst type of peripheral nerve damage (called neurotmesis) involves complete division of a nerve, including all the microscopic tubes and surrounding tissues that support the nerve. This can happen with extreme stretching of the nerve that causes the nerve to snap, or if the nerve is cut by the sharp edge of a broken bone, or following a stab injury. With the nerve in two pieces, there is no hope for the regenerating nerve fibres to find their way without surgery to repair the nerve ends.
“Peripheral nerve surgery can help improve function in the most severe nerve injuries, although full recovery is rarely if ever achievable.”
Peripheral nerve injuries that I see and treat include:
Median nerve injury, for example after a deep cut of the wrist
Radial nerve injury, for example after a fracture
Ulnar nerve injury, for example after an elbow injury
Axillary nerve injury, for example after a shoulder dislocation
Common peroneal nerve injury, for example after knee ligament damage
Long thoracic nerve injury, associated with winging of the scapula.
Determining the severity of a nerve injury can be surprisingly challenging. I will usually use information from scans, electrical nerve conduction studies and electrical measurements from muscles to help decide whether a nerve injury is better left alone to recover without surgery.
Although sensation can be partially regained even years after the original injury, muscles gradually become unreceptive to nerve regrowth sometime between 12 and 24 months following injury. This change in the muscle is permanent, therefore it is my priority to get nerve to muscle quickly in order to preserve as much muscle function as possible.

“Time is very much of the essence when treating nerve injuries”
Reconstructive nerve surgery
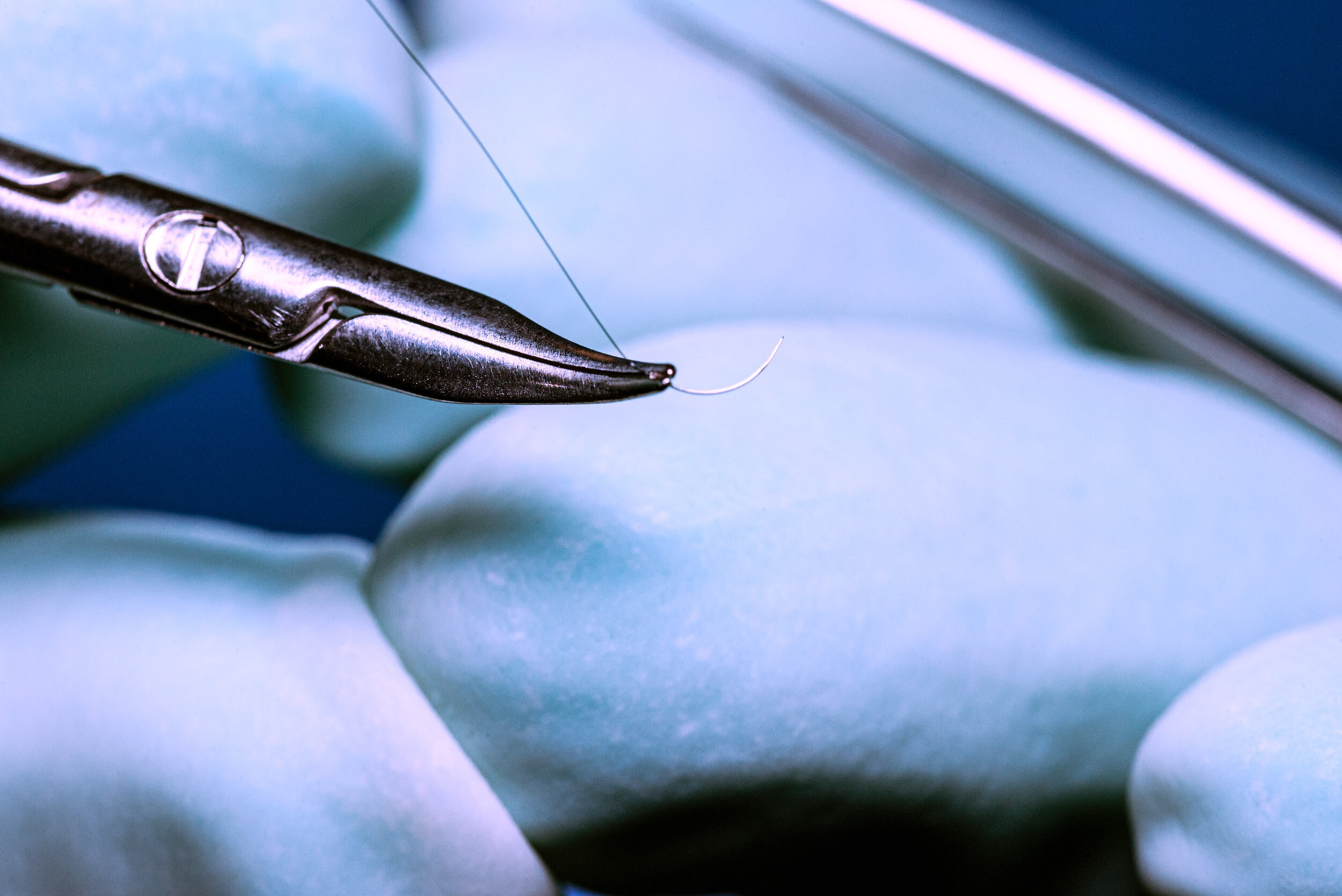
There are many different types of reconstructive nerve surgery; I select the technique that offers the best chance of recovery based on the circumstances. If possible, the nerve is repaired by stitching both ends back together. This is done under magnification using an operating microscope, in order to align the ends of the nerve as closely as possible to their original position. This will help guide the regenerating nerve fibres back to their intended targets in the skin or muscle. A nerve repair is usually possible if done within a few days after a sharp injury, such as after a knife wound.
If the nerve is stretched or crushed in two, the unhealthy damaged nerve endings have to be cut back and this produces a gap between the nerve ends. In these cases, a nerve graft is used to bridge the gap and encourage the nerve fibres to grow across the site of injury. Not all the nerve fibres make it across because they have to get through two joins at each end of the nerve graft, but some useful functional recovery is possible.
The nerve graft is taken from other parts of the body, using small ‘non-critical’ sensory nerves, such as the sural nerve that gives sensation to the outer border of the foot, or a nerve that gives sensation to the inner surface of the forearm. Once these nerves have been taken for use as a graft, the area they supply become permanently numb. The technique is a trade-off between causing an area of numbness in a ‘non-critical’ area versus trying to regain function in a more important area, such as thumb movement and sensation.
In some cases, where muscle recovery is not expected for a very long time (for example, if a nerve to the hand is injured high up in the neck), a nerve transfer may be used. This technique takes an uninjured nerve that lies close to the target muscle, and transfers it to the injured nerve at that level. This gives a short-cut pathway to the muscles that bypasses the site of original injury, allowing nerve to grow into muscle much sooner – before it becomes unreceptive to nerve regrowth.
Nerve compression
Nerve compression injury results from muscles or sinews in the arms or legs becoming tight and squeezing a nerve. Usually the cause is not known. Sometimes an area of scarring around a nerve following an injury or previous surgery can tighten around a nerve or tether it so it kinks.
“Nerve compression can cause tingling pins and needles, numbness, pain or even muscle paralysis – similar to what happens if you sit on your leg for too long.”
Some nerve compression conditions, such as carpal tunnel syndrome at the wrist, can sometimes be treated with non-surgical interventions such as a steroid injection or a splint. Sometimes it is simply a case of avoiding placing pressure on the nerve, such as not leaning your elbow with the ‘funny bone’ on the windowsill when driving.
If symptoms are bad enough and have not responded to these simple treatments, a nerve can be surgically decompressed by cutting the compressive band of sinew or removing the region of constriction that is squeezing the nerve. If there is scarring or tethering around a nerve, this can be carefully cut away under a microscope in a procedure called neurolysis. Once the release has been performed, how quickly the nerve returns to normal depends on how much damage has been done by long-term compression.
Mild cases regain normal function within a matter of minutes of the surgical release as the blood flow to the nerve returns to normal levels. More severe compression not only has the blood squeezed out of the nerve but also the insulation material around each nerve fibre breaks down. After decompression, the nerve has to regenerate this insulation before it starts working properly – this can take several months.
In extreme cases, not only has the nerve insulation broken down, but the nerve fibre itself is disrupted due to long-term pressure. Recovery is theoretically possible if the nerve fibre can regrow from the point of compression to its target skin and muscle, but this takes many months. Unfortunately, in long-standing cases, the processes that cause nerve damage also cause internal scarring within the nerve, which makes full recovery impossible.
Examples of nerve compression syndromes that I see and treat include:
Carpal tunnel syndrome (wrist)
Cubital tunnel syndrome (elbow)
Common peroneal nerve compression (knee)
Guyon’s canal (ulnar nerve at the wrist)
Lacertus syndrome (median nerve at the elbow)
Pronator syndrome (median nerve in the forearm)
Superficial peroneal nerve compression (calf)
Wartenberg’s syndrome (superficial radial nerve in the forearm)
Meralgia paraesthetica (lateral cutaneous nerve of the thigh at the hip)
Radial tunnel syndrome (forearm)
Tarsal tunnels syndrome (ankle)
Long thoracic nerve compression (winging shoulder blade)
Thoracic outlet syndrome (brachial plexus in the neck)
Except for carpal and cubital tunnel syndrome, most of these conditions are rare. However, following a severe nerve injury, a recovering or regenerating nerve can be impeded at predictable anatomical ‘pinch points’. This can produce a tingling sensation when the pinch points are lightly tapped. If nerve recovery has stalled, sometimes decompressing the pinch points can relieve an obstruction that allows the regenerating nerve to continue on its journey to its target.
Nerve tumours
There are different types of peripheral nerve tumour, and their treatment requires more assessment and planning than other simple lumps. They may be benign or malignant; some are associated with a syndrome such as neurofibromatosis. Patients usually notice a lump, but may also complain of symptoms of nerve compression – a variable mixture of pins and needles, numbness, pain and muscle paralysis.
A schwannoma – also known as a nerve sheath tumour – grows from the microscopic layer of tissue that surrounds the nerve fibres. As it grows it pushes on the nerve fibres, causing symptoms. Using a microscope, it is often possible to cut between the nerve fibres to remove a schwannoma from inside a nerve without causing much lasting nerve damage.
In contrast, a different type of nerve tumour called a neurofibroma grows in a more haphazard way and incorporates other cell types including nerve fibres. The resulting tumour is a mishmash of tumour and nerve fibres that cannot be separated, even under an operating microscope. If a neurofibroma is causing troublesome symptoms it can be removed, but unlike a schwannoma, removing a neurofibroma also means removing the nerve.
If the neurofibroma is growing within a tiny nerve branch to a patch of skin, then removing the nerve may not cause any noticeable loss of sensation. However, if the neurofibroma is within a major nerve, removal may cause significant areas of numbness, weakness and pain. The decision to operate is therefore not taken lightly and it may be preferable to monitor or observe such tumours.
“If a nerve has to be removed, nerve transfers or nerve grafting can be used to restore some function.”
Scans, such as ultrasound or MRI, can suggest whether a nerve tumour is likely to be a schwannoma or neurofibroma, but the only way to be sure is to remove some of the tumour for analysis.
I send most cases of nerve tumour to a specialist sarcoma multidisciplinary team for their combined opinion. They will assess all available information and scans and advise whether the tumour can be treated as a benign tumour or if there are suspicious features that require more specialised scans. A malignant peripheral nerve sheath tumour is a rare but aggressive tumour that requires surgical removal by a sarcoma surgeon, who specialises in treatment of these rare malignancies.
Nerve pain
Peripheral nerve pain, or neuropathic pain, is a complex topic. Different pain experts argue about the best way to treat neuropathic pain, and some experts believe that surgery should never be done for nerve pain. In contrast, many nerve surgery experts (myself included) have personal experience of curing someone’s nerve pain through surgery.
The problem is that not everyone I operate on ends up pain-free in the long run, and it is very difficult to select which patients will improve and which won’t. I will explain the decision-making process to you, so that you understand the uncertainties that exist in peripheral nerve pain treatment to make sure we make the right decision about your further treatment together.
Nerve pain can be severe, and patients often use these words to describe the pain:
Burning
Stabbing
Tingling
Twisting
Squeezing
Cramping
Cutting
Shooting
Numbing
Stinging
Pulling.
Nerve pain can occur after a nerve injury, where the cut nerve ending forms a neuroma.
“A neuroma is a bundle of raw, sprouting nerve endings surrounded in scar – a bit like an extremely sensitive head of cauliflower.”
Repairing a nerve at the time of injury can help prevent a neuroma by giving the cut nerve ends a pathway to grow away from the injury site towards its targets in muscle or skin. However, if a nerve is cut when performing an amputation of a leg, the other end of the nerve is not available so nerve repair is not an option and a neuroma is inevitable. Nerve pain can also arise from nerve compression or nerve tumours; releasing the nerve or removing the tumour can help improve the pain.
It is important to determine where the nerve pain is coming from. Nerve pain in the hand may come from a nerve injury within the hand, or from the nerve as it travels through the forearm, or even from an injury in the neck. Decompressing a nerve in the hand will have no effect if the cause of the pain is coming from the neck.

I use various clinical tests, scans, electrical nerve tests and ultrasound-guided nerve injections to get as much information as possible about the location of the problem so the surgery can be targeted.
If a neuroma at the wrist is causing severe pain when touched by the cuff of a shirt or wristwatch, I can remove the neuroma and move the end of the nerve up the forearm. Although a neuroma will re-form, the aim is for the neuroma to be smaller and better-padded than before so it stops causing as much of an issue. If both ends of the nerve can be found, then after cutting back the neuroma the gap can be bridged using a nerve graft in the hope that the nerve will grow down the graft rather than forming another neuroma.
“The outcomes of operating on painful nerves can be unpredictable, and for that reason I prefer to treat the most complex pain problems in a team of like-minded colleagues and physiotherapists with a specialist pain management background.”
If severe pain has been present for many years, pain pathways in the brain become established and ‘centralised’, so that even if the neuroma is removed, the brain or spinal cord continues to generate pain signals. This can be frustrating for me and for the poor patient, who has gone through surgery for little benefit. In a situation where all surgery and medication treatment has failed to help, a pain specialist may suggest a pain management programme.
Parsonage-Turner syndrome
This condition is also known as brachial neuritis or neuralgic amyotrophy. It is a peripheral nerve disorder that causes severe pain, usually involving the shoulder and arm. The pain is followed by weakness or paralysis in these areas. In most cases, the cause is unclear but the commonest theory is that a mild viral illness triggers an immune response to certain nerves.
The vast majority of patients with Parsonage-Turner syndrome recover on their own without any treatment, with spontaneous return of muscle strength and resolution of pain. While awaiting recovery, it is important to move and exercise the affected limb under the guidance of a physiotherapist. Special pain killers that target nerve pain can also help. Surgery is rarely required, but can help improve recovery if nerve recovery stalls at predictable pinch-points.

“After I met with Mr Dafydd I was put at ease and reassured that he would do his best to sort out the problem.”
— Jeremy, 55. Peroneal nerve patient